Medicaid: A Lifeline for Recovery
For many people in recovery with opioid use disorder (OUD), Medicaid is not a privilege, it’s a lifeline. Medicaid provides essential coverage for addiction treatment, counseling and medication. Without it, continuous care is interrupted, and lives are put at risk.
What is Medicaid?
Medicaid is a joint federal–state health insurance program. The program covers people with low incomes and also includes pregnant individuals, children and people with certain disabilities. For those with OUD, Medicaid often covers:
- Medication for opioid use disorder (MOUD), such as buprenorphine and methadone, and sometimes long-acting injectables
- Counseling and outpatient treatment programs
- Hospital and emergency care
- Other essential health services (mental health, primary care, substance use disorder counseling, etc.)
Medication-assisted treatment (MAT) uses medications approved by the U.S. Food and Drug Administration (FDA) in combination with counseling and behavioral therapies to treat OUD.
Medicaid Coverage is Vital to Beat the Opioid Epidemic
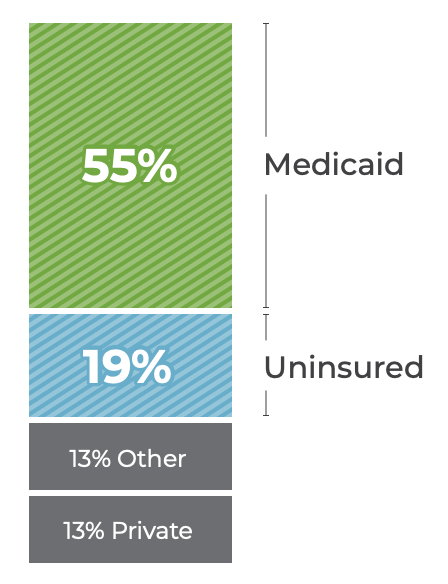
Medicaid is the largest payor of substance use disorder treatment in the country and a lifeline for people in recovery.
- 55% of the OUD patient population uses Medicaid to cover treatment costs. (KFF)
- MAT leads to $25,000-$105,000 in lifetime savings per person. (NIH)
- States that expanded Medicaid saw a 6% reduction in overdose deaths. (JAMA Network)
Why Continuous Care Matters
The evidence is clear. Interruptions in coverage or treatment are not safe. They lead to higher risks of relapse, overdose and death.
- A recent meta-analysis found that MAT reduces opioid‐related mortality by about 50% compared to no medication treatment. (American Heart Journal Plus: Cardiology Research and Practice)
- In one large cohort study of patients hospitalized with an OUD-related diagnosis (over 22,000 people), those who initiated MOUD within seven days after discharge had significantly lower odds of fatal or nonfatal overdose in the following six months (adjusted odds ratio ~0.63). (JAMA Network)
- Another study involving formerly incarcerated individuals showed that Medicaid expansion in Rhode Island was associated with sustained decreases in all-cause mortality, including overdose mortality, compared to a control state without expansion. (JAMA Network)
Continuous coverage is therefore not optional, it is essential. Gaps in treatment or insurance create life-threatening risks.
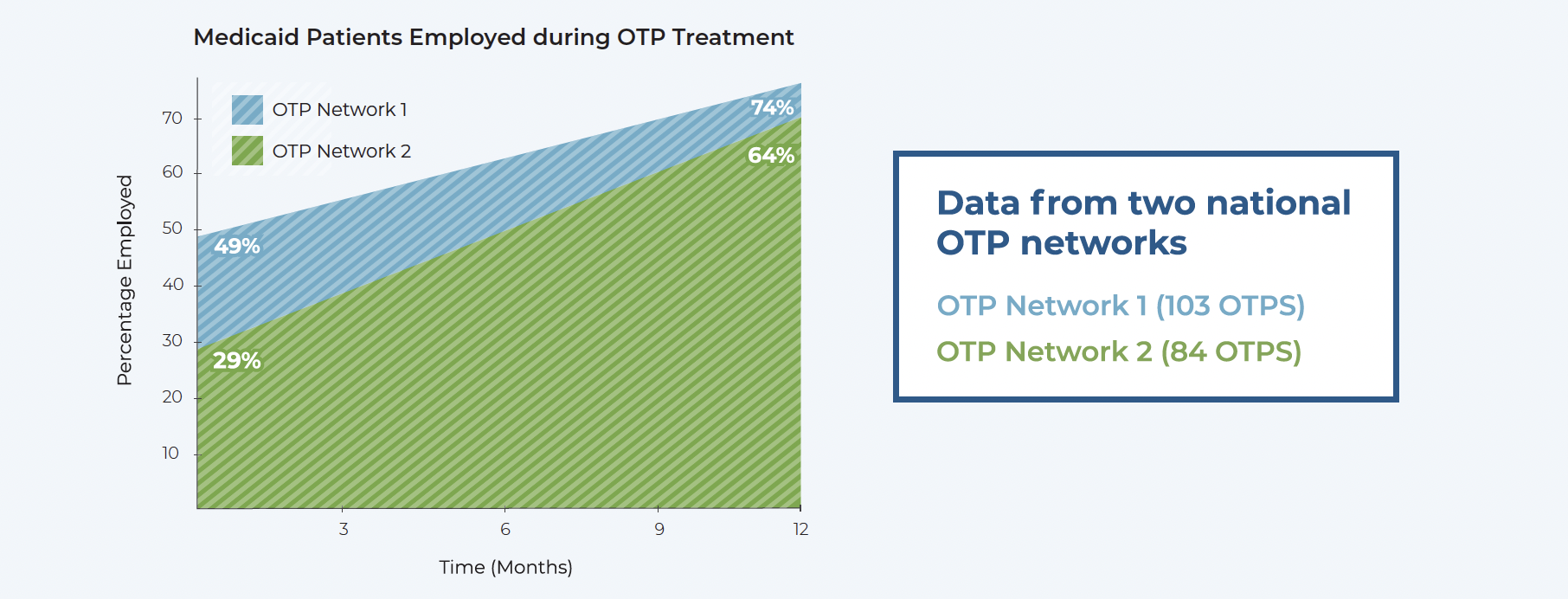
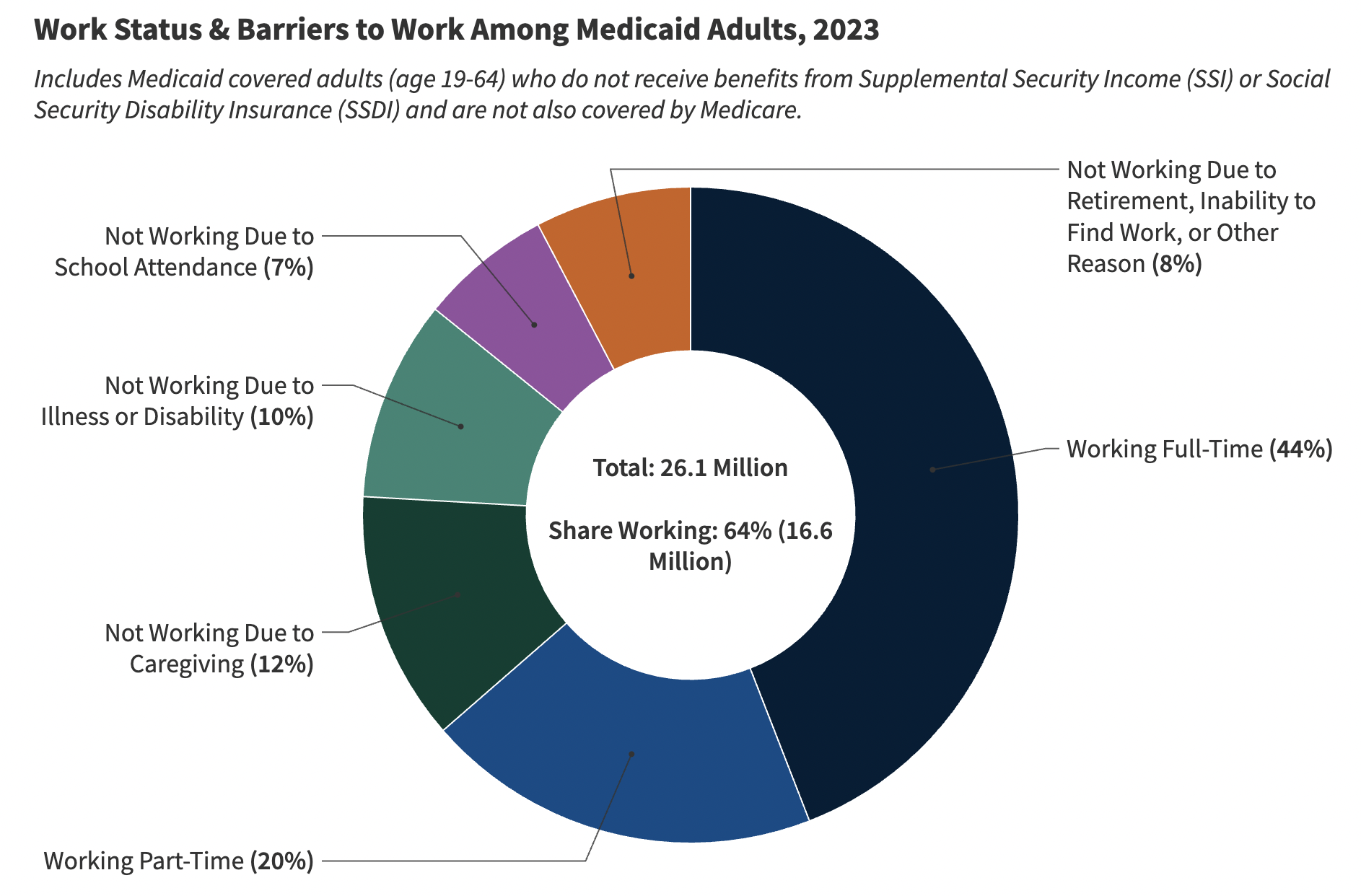
MAT Leads to Employment
Continuity of treatment reduces overdose risk, improves outcomes, promotes strong communities and families, and increases employment stability, which ultimately reduces long-term Medicaid reliance. Burke, Sullivan, et al. (2022) found that individuals receiving MAT had higher employment rates and earnings compared to those not receiving MAT (Federal Reserve Bank of Boston). A representative sample of our members’ data validates that this correlation is unequivocally true for Medicaid patients.
Barriers that Put Recovery at Risk
Work Requirements and Housing-Related Barriers
When patients begin MAT, they are in crisis— experiencing severe and painful withdrawal symptoms, often in legal trouble and isolated from family and friends. Most are not stable enough to secure and maintain a job. A goal of treatment is to stabilize the patient, which then allows them to secure employment, return to school or enroll in job training. Sustained Medicaid coverage is vital during this critical time. It is in the best interest of patients, communities and society to encourage patients living with OUD to stay in treatment.
Co-Pays and Cost Sharing
Even small fees deter people from maintaining treatment, filling prescriptions or accessing counseling. For people managing recovery and unstable finances, these costs can mean missed doses or treatment interruptions—risks that can be fatal. For individuals in recovery, these barriers are especially harmful. Recovery often involves frequent clinic visits, unstable housing, health issues that limit consistent employment, and other challenges that make rigid work requirements or cost burdens unrealistic.
Call to Action
Congress passed the One Big Beautiful Bill Act (OBBBA) in 2025, which established community engagement requirements for Medicaid beneficiaries that will go into effect in January 2027. Because federal policymakers understand the unique challenges of addiction treatment and recovery, people living with substance use disorder were exempted from work requirements and co-pays. These exemptions are critical to ensuring people with OUD have continuous coverage so they can remain in treatment; however, it remains to be seen how states will implement the community engagement requirements. These exemptions are necessary, and each state must work with Centers for Medicare & Medicaid Services (CMS) to develop exemption processes that are easy to follow and not punitive.
Policy must reflect reality: people in treatment need stability, not red tape.
- State regulations should ensure the federal sense of Congress is honored: that exemptions exist, are easy to access and truly protect people in treatment
- Exemptions must not be punitive or bureaucratic, they should safeguard access to continuous care
Watch Jodie’s Story:
Jodie Shares the Importance of Therapy in Recovery
Progress is Being Made in Fighting the Opioid Crisis
Data from the Centers for Disease Control and Prevention (CDC) suggests a possible connection between increased access to MAT and a 19% drop in overdose deaths between July 2023 and 2024.
There are no silver bullets to this complex problem, but progress directly correlates to expanded access to Opioid Treatment Programs (OTPs) and all forms of medication-assisted treatment (MAT), made possible by reforms enacted by Congress and the Substance Abuse and Mental Health Services Administration (SAMHSA).
The 2018 SUPPORT Act created access to MAT in OTPs for Medicare beneficiaries. It also temporarily required state Medicaid programs to cover MAT—a provision made permanent by Congress in 2024. These changes dramatically improved access to OTPs.
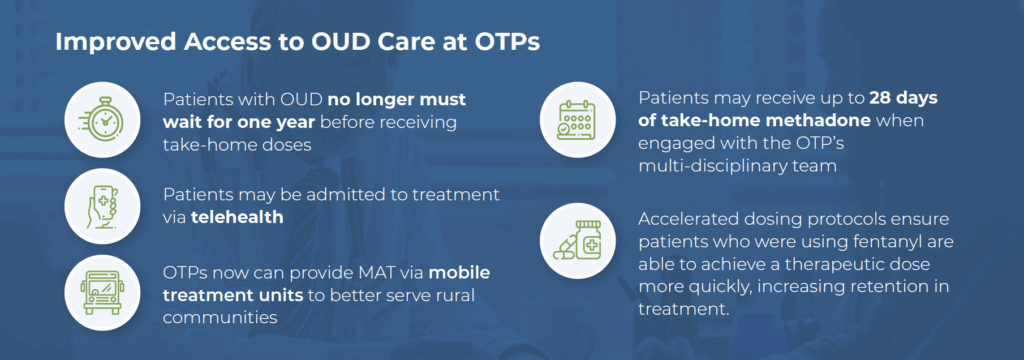
SAMHSA and the Drug Enforcement Administration (DEA) recently made permanent important regulatory flexibilities that have helped people stay in treatment. (CDC).